Hi CashireCat,
I was not so lucky with my therapist... I had the pelvic floor training at that time only in the context of the rehab - and that was not particularly individual and took place in a group...
Anyway - as far as the neurologist is concerned - I would take a closer look again. I don't know how it is in the States - but here in Germany there are clinics with special continence centers where urologists, neurologists, gynecologists and proctologists work together.
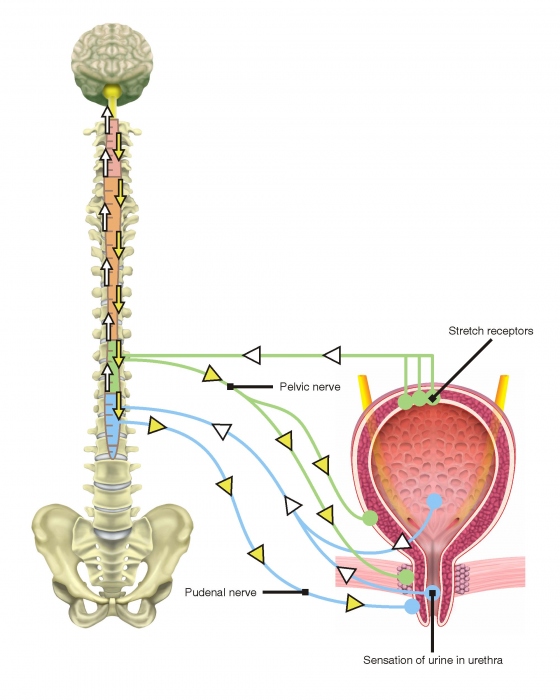
I also went to a neurologist first as it figured out that also a neurological problems my the reason for my continence problems. The neurologist did all kinds of tests but found nothing really significant. I only really got further in the continence center. Maybe it's different for you - but the problem with neurologists is that they normaly can only measure the large nerve tracts. If peripheral body parts (legs / arms) are affected, they usually find something. But if the autonomic nervous system and internal organs are affected, it is more difficult and special knowledge not only about the nerves but also about the affected organs is needed.
I think you have to make a very differentiated diagnosis to be able to distinguish between the things. In my case, it is also a multifactorial problem - and I lost a lot of time while several specialists try to work on it separately. In fact there are several thinks that may work even with neurological issues - depending on the problem you might be e.g. a candidate for an interstim.